The goal of this CE activity is to provide nurses and nurse practitioners with knowledge and skills to manage patients on anticoagulant drugs. After reading this article, you will be able to:
- Identify common indications for use of anticoagulants
- Describe monitoring requirements
- Consider important safety implications to help prevent complications
- Discuss patient/family educational needs related to anticoagulants
Authors: Dana Moore, MS, RN, CSHA Regina Hendrix, MSN, MPA, RN-BC Deena Conti, BSN, RN Felix Guzman, BSN, RN
 Anticoagulation medications are high-risk drugs.1 There is a very small window for therapeutic dosing: too much of a drug can cause bleeding, and too little may lead to clotting. In 2008, The Joint Commission published a new National Patient Safety Goal (NPSG) to address high-risk anticoagulation drugs used for treatment. This Goal, with an implementation date of January 2009, required organizations to develop and implement standardized practices in order to reduce harm. While the NPSG applies to all anticoagulants, this educational offering will focus on the most commonly used anticoagulants: unfractionated heparin (UFH), low molecular weight heparin (LMWH), and warfarin.
Anticoagulation medications are high-risk drugs.1 There is a very small window for therapeutic dosing: too much of a drug can cause bleeding, and too little may lead to clotting. In 2008, The Joint Commission published a new National Patient Safety Goal (NPSG) to address high-risk anticoagulation drugs used for treatment. This Goal, with an implementation date of January 2009, required organizations to develop and implement standardized practices in order to reduce harm. While the NPSG applies to all anticoagulants, this educational offering will focus on the most commonly used anticoagulants: unfractionated heparin (UFH), low molecular weight heparin (LMWH), and warfarin.
Monitoring and Safety Implications
Heparin requires close monitoring because of its narrow therapeutic index, increased risk for bleeding, and potential for heparin-induced thrombocytopenia (HIT). Monitoring includes thorough head-to-toe patient assessments for potential side effects, and laboratory monitoring.
Bleeding is the most common side effect, and may present in a variety of ways: epistaxis, gum bleeding, hemoptysis, hematuria, melena or hemorrhage. Undiagnosed and uncontrolled bleeding may lead to cardiovascular collapse or cardiac tamponade. In the event of major bleeding, heparin should be stopped, and, if necessary, protamine sulfate may be administered.
Heparin-induced thrombocytopenia (HIT) is an antibody-mediated reaction characterized by a profound decrease in platelets—typically a 50% reduction in the platelets from baseline2—within 5 to 10 days after exposure to heparin. It is a potentially life-threatening condition and causes thrombosis in approximately 50% of affected patients. Treatment involves discontinuation of all heparin products (including flushes) and administration of a non-heparin anticoagulant. Providers should carefully document history of HIT and the medical record, and patients should be educated to inform all providers of HIT history.
Laboratory monitoring typically includes measurements of coagulations, such as activated partial thromboplastin time (aPTT), prothrombin time (PT), plasma heparin concentration (antifactor UFH Xa), whole blood clotting time, activated clotting time, plus a complete blood count (CBC) to monitor platelets and assess for bleeding. The aPTT is most commonly used as a global measure of a patient’s overall anticoagulation. Each institution defines its own therapeutic range, typically, 1.5 to 2.5 times the control aPTT. It is important to note aPTT is an indirect measurement of heparin’s therapeutic effect; therefore, aPTT levels can be affected by numerous biological factors such as lupus anticoagulants, factor XII deficiency, elevated procoagulant factor VIII, oral anticoagulants, liver diseases, and medication interactions. Also, aPTT may be affected by the reagent used to perform the test; there may be variation in aPTT across institutions secondary to the reagent used. It is important to note there is a strong link between sub-therapeutic aPTT values and recurring thromboembolism; at the other end of the spectrum, there is a 7% increase in the chance of bleeding for every 10-second increase in the aPTT, even when the aPTT does not exceed 100 seconds.3
The anti-Xa assay is an alternate laboratory measurement for anticoagu-lation. This assay is a direct measure of heparin activity and works by measuring the ability of heparin-bound antithrombin (AT) to inhibit a single enzyme, Factor Xa. The therapeutic range for anti-Xa UHF activity is 0.3 to 0.7 international units of heparin per milliliter. High values indicate high levels of heparin; low values indicate low levels of heparin. It has minimal interference from biological factors discussed above, but our Johns Hopkins Hospital (JHH) experience suggests a small number of patients have normal anti-Xa UFH assays with an elevated aPTT. Due to bleeding risks, a combination of both tests may be beneficial in patients with complex illness.
Nurse-driven heparin nomograms for IV heparin administration are used at JHH to manage many adult patients’ anticoagulation needs. Providers order a heparin therapy anticoagulation target, and nurses use a clinical algorithm to guide care. Nurses obtain baseline labs; calculate and administer initial bolus dose; order and evaluate anticoagulation labs; and titrate heparin to therapeutic goal based on clinical algorithm and patient presentation. Laboratory monitoring involves obtaining and evaluating labs every 6 hours post a dose change until two consecutive anticoagulation lab results are within target. Once target anticoagulation is achieved, anticoagulation labs are monitored once daily.
Patient Education
Patients on anticoagulant therapy must be educated about their increased risk for bleeding, monitoring for bleeding, managing bleeding if it occurs, and drug-specific information.
Low Molecular Weight Heparin (LMWH)
Indication
Low Molecular Weight Heparin (LMWH), like UFH, is used for treat-ment and prevention of VTE. There are several advantages of LMWH over UFH: longer half-life, higher bioavailability, a predictable dose response, and decreased risk for HIT. Dosing is based on patient weight, administration schedule, and patient-specific considerations.
 Monitoring and Safety Implications
Monitoring and Safety Implications
Nursing assessment for the patient on LMWH is the same as for the patient on UFH; however, laboratory monitoring is rarely required.4 Anti-Xa LMWH monitoring may be warranted for specific patient conditions: obesity (BMI greater than 50 kg/m2); small stature (less than 50 kg); impaired renal function (creatinine clearance less than 30mL/min); and pregnancy. The anti-Xa laboratory test for LMWH is different from the anti-Xa laboratory test for UFH; target (peak) ranges for anti-Xa LMWH are approximately 0.6 to 1.0.5
LMWH dosing should be adjusted if the anti-Xa is not in the desired target range per provider order.
When transitioning from a heparin infusion to subcutaneous LMWH, discontinue the infusion concurrently with the first dose of LMWH.
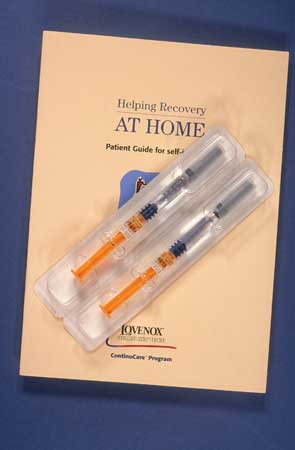
Patient Education
Patient education needs are similar to those of UFH. In addition, patients who will self-administer LMWH must be instructed on correct subcutaneous administration technique.
Warfarin (Coumadin)
Indication
Warfarin has similar clinical indications to UFH. It is available in both IV and oral formulations, but is most commonly used as an oral anticoagulant. It is preferred to UFH and LMWH when a patient requires long-term anticoagulation.
Monitoring and Safety Implications
Warfarin has a narrow therapeutic index, so monitoring includes assessment for potential side effects, laboratory tests for dose titration, and vigilance for potential drug and food interactions.
Bleeding is the most common side effect, most frequently in the GI tract. Warfarin may cause skin necrosis, or cholesterol embolus syndrome. Specific patient variables may impact drug metabolism. For example, active hepatic disease, certain drugs, and old age are likely to enhance the response to warfarin.
The International Normalized Ratio (INR) is the recommended method for monitoring warfarin, and the target goal is set by the provider, based on clinical indication. An INR goal of 2 to 3 may be appropriate for treatment or prevention on thromboembolism; higher targets of 2.5 to 3.5 may be appropriate for high-risk patients.6 Baseline INR and CBC should be obtained prior to initiation of warfarin therapy, and reassessed until the therapeutic range has been reached. It can take 2-3 days for the INR to reflect a change in the dosage, so daily increases in the dose to meet the target goal are usually not appropriate. If a patient is transitioning from IV heparin to PO warfarin, heparin should be continued for at least 24 hours after the INR reaches the ordered target range. Daily monitoring of PT/INR and aPTT is recommended for patients concurrently on heparin and warfarin.
Warfarin has many potential drug and food interactions. Commonly prescribed drugs that may increase anticoagulation and INR include: acetaminophen, metronidazole, sulfamethoxalone, and omeprazole. Foods containing vitamin K may decrease anticoagulation and INR.
Patient Education
Patient education topics for the patient on warfarin include medication adherence, INR target, importance of laboratory monitoring, and necessity of communicating changes in their medication regime to health-care provider. Diet education is critical, particularly for foods that contain vitamin K. The patient does not need to avoid foods rich in vitamin K, but the patient must be consistent with consumption habits.
Conclusion
Anticoagulation drugs can be life-saving. Nurses must carefully assess, closely monitor, and comprehensively educate the patient receiving anticoagulation drugs to ensure the full benefit of anticoagulation therapy and to minimize potential harm.